How AI can solve the Healthcare labor shortage epidemic
Healthcare is the industry that AI can change the most, improving our lifes dramatically. This is how we start
Hey everybody! I was super lucky to get Lucía Vives, founder of Youshift to write for us about here vision about the future of Healthcare.
I invested in Youshift some months ago after just one meeting with Lucía.
The sheer amount of talent and drive these founders have is amazing, as well as their market knowledge and experience (all three of them are Harvard grads).
PS: If you want to reach out to Lucía you can do so here.
Enjoy!
I grew up in Spain in a family of doctors. I was fascinated by medicine, but I knew I didn’t want the life that came with it. So I studied Biomedical Science, convinced I could stay close to healthcare while choosing a different path.
In my third year of college, at Harvard, I met my two co-founders: Jota Chamorro and Adolfo Roquero. Both engineers. Both from families of physicians. We didn’t set out to start a company. We set out to understand why one of the most fundamental systems in healthcare, workforce management, is still broken.
If you know this industry, I hope you read what follows with care.
If you don’t, I hope you read it anyway.
What’s happening to the healthcare workforce isn’t isolated to one hospital system or one country. It is structural, and it will affect all of us, globally, if we don’t build better infrastructure.
Where we are heading
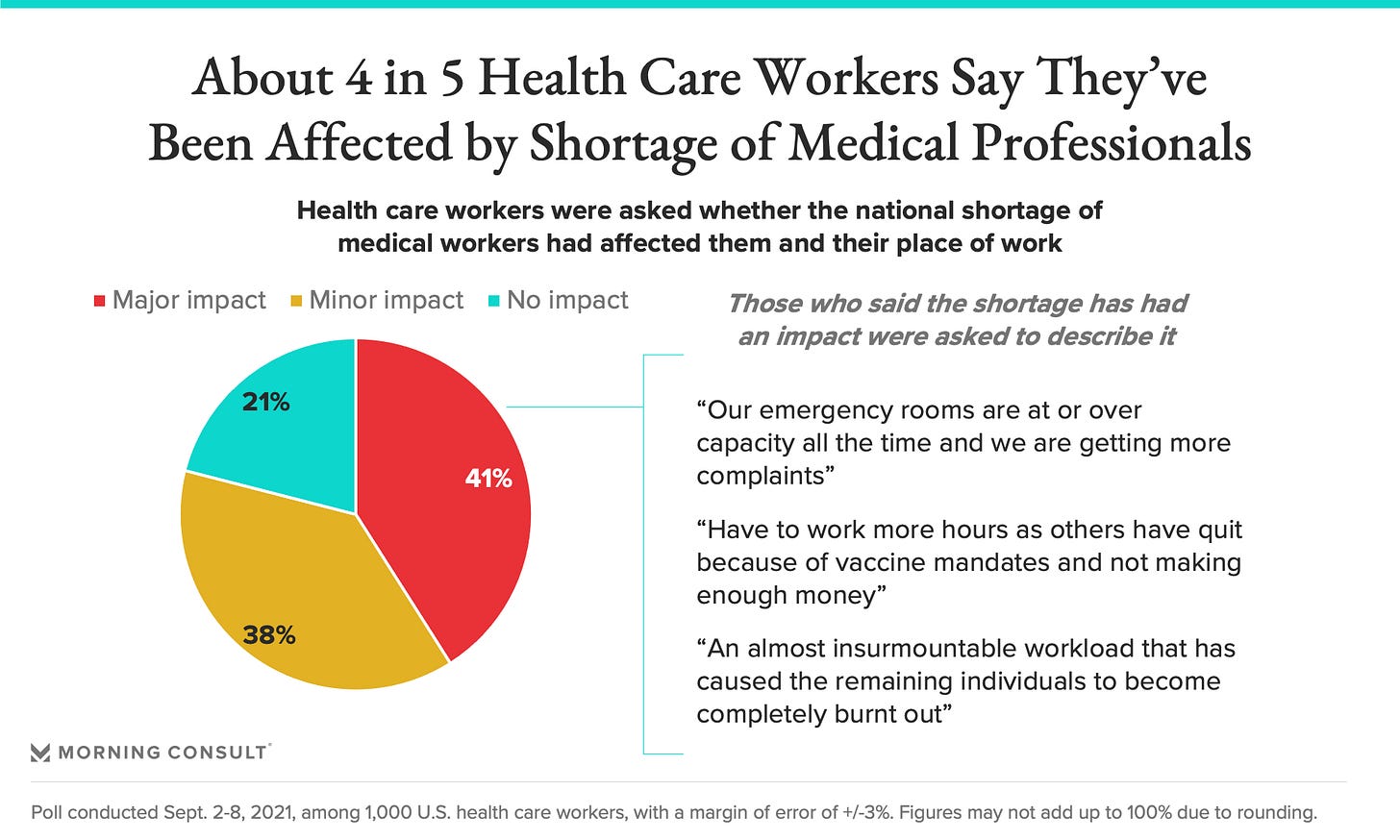
Healthcare is facing the worst labor shortage.
By 2033, the US alone is projected to face a shortage of more than 100,000 physicians and 200,000 nurses, nearly 10% of the clinical workforce. At the same time, the population over 65 will grow by more than 40%, inpatient demand is projected to rise by at least 10%, and 49% of physicians report burnout.
Meanwhile, labor expenses increased by $42.5 billion in just two years, and now represent nearly 60% of hospital operating costs.
So we have a system where the main input (clinicians) is shrinking, the main demand driver (aging population) is expanding, and the main cost center (labor) is under unprecedented pressure.
When hospitals cannot staff shifts, they buy relief.
Last year alone, US health systems spent over $10 billion on temporary clinicians, often paying 30–50% more per shift. But the deeper issue is not just cost, it’s incentives.
While hospitals are trying to build stable, long-term clinical teams, temporary staffing markets are structured around filling recurring short-term gaps. Higher short-term pay naturally pulls clinicians toward temporary assignments instead of permanent roles, and contractual restrictions can make it harder for those clinicians to transition into full-time positions at the hospitals where they work. In a labor market that is already supply-constrained, this dynamic fragments the workforce further.
And yet, the system that coordinates all of this — who works, when, at what cost, under which constraints — is still managed through legacy software, spreadsheets, manual workarounds, and large administrative teams. In fact, workforce management has become so complex that many hospitals outsource entire departments to specialized companies.
The impact of solving this problem
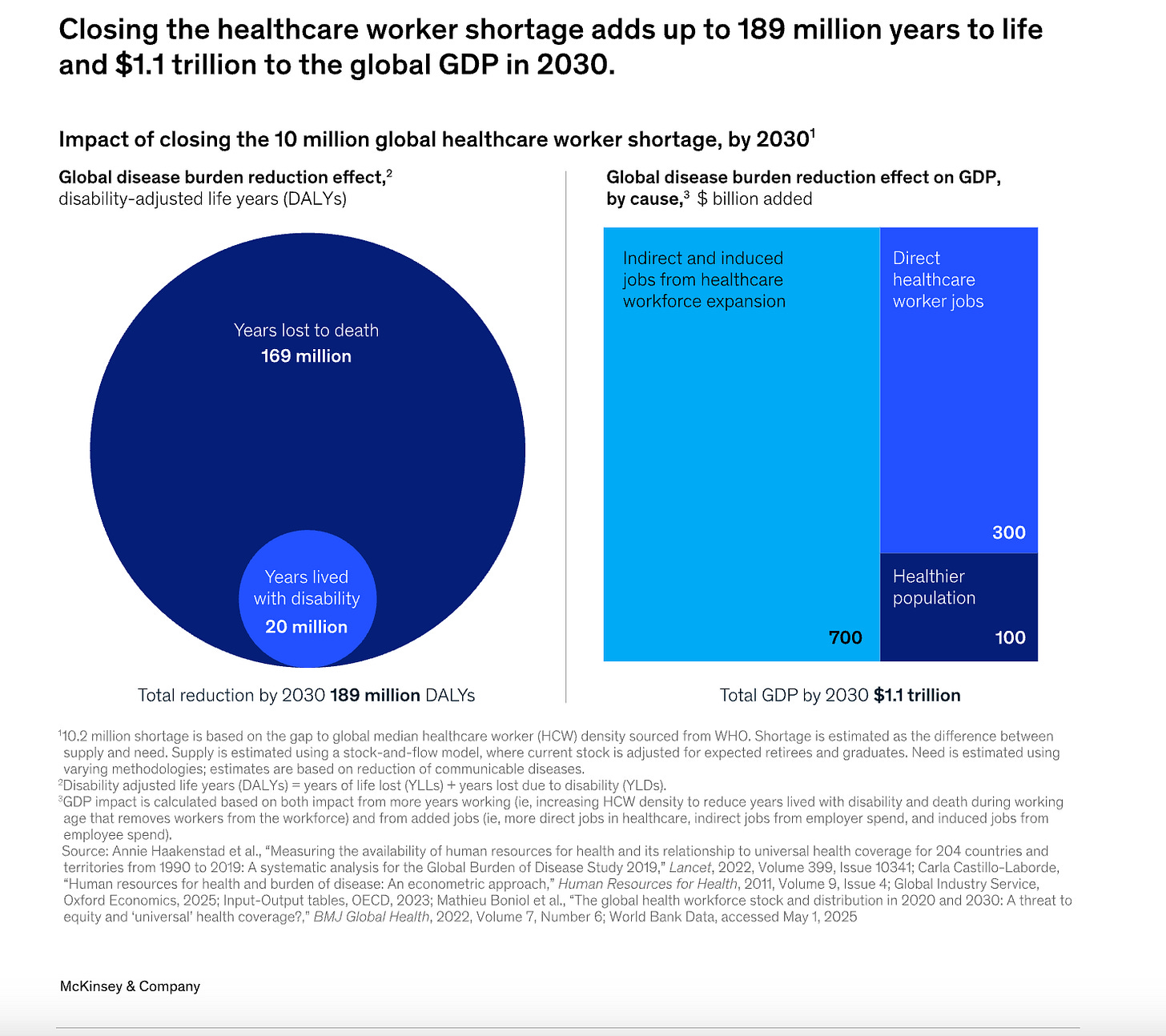
Solving the global healthcare labor shortage (at least 10 million workers by 2030) would be one of the highest-leverage “infrastructure” upgrades society can make: McKinsey Health Institute estimates it could eliminate about 7% of the world’s total disease burden by enabling more timely access to essential services (from maternal care to chronic disease management), averting ~189 million years of life lost to early death and disability, and lifting global life expectancy by roughly 1.5 years on average (with much larger gains in the hardest-hit regions, especially Africa, which holds ~52% of the shortage and 70%+ of the opportunity to reduce disease burden, where life expectancy could rise by ~7 years).
Economically, closing the gap could add around $1.1 trillion to global GDP in 2030, partly through the direct creation of healthcare jobs (~$300B) but mostly through second-order effects: a healthier population and workforce that boosts productivity and indirectly creates jobs beyond healthcare, meaning this is not just filling vacancies, but unlocking better health, faster care, and broad-based growth at global scale.
The first step: solving staffing
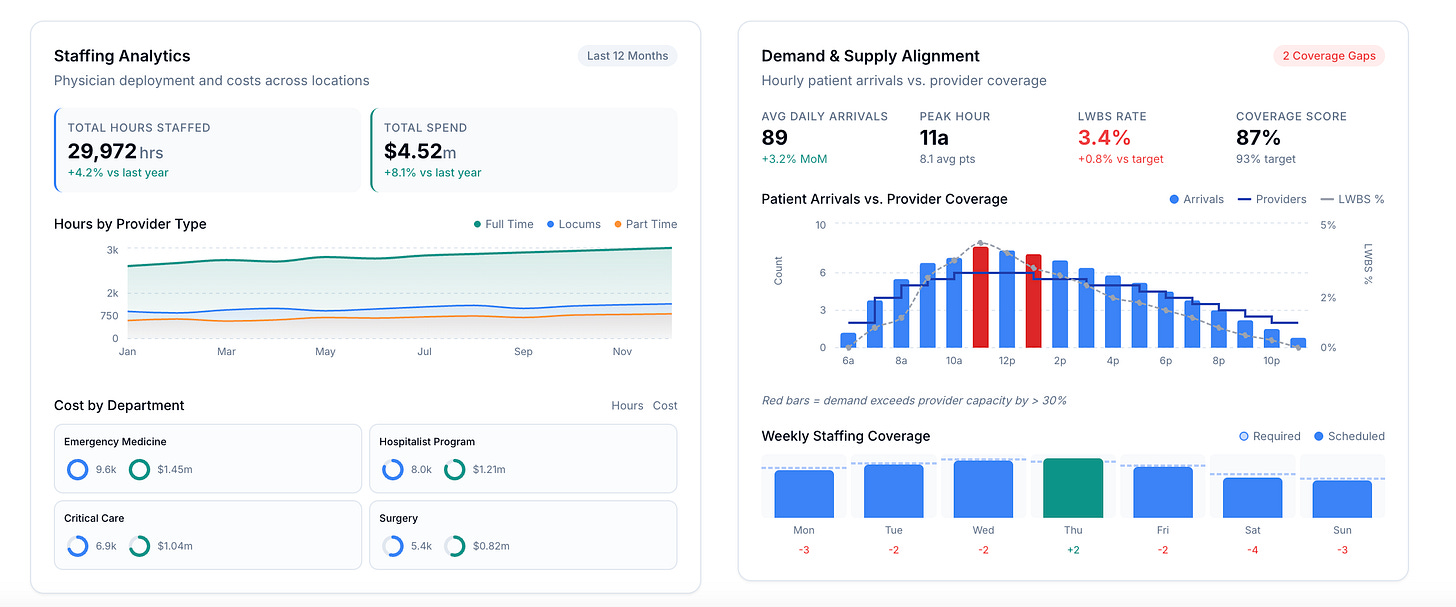
Today, about 60% of U.S. emergency rooms are staffed by physician groups. Their profitability depends almost entirely on how efficiently they manage labor. And yet, even at this level of scale and specialization, they lack a true operating system built for it.
Either we redesign how healthcare labor is managed, with precision, intelligence, and scale, or the infrastructure behind care will continue to erode under pressure.
When we stepped back and examined the system more closely, it became clear that workforce management in healthcare fails in two fundamental ways.
First, there is no true optimization.
Staffing a hospital is a constrained, multi-objective allocation problem. Every schedule must balance clinical coverage, legal requirements, compensation structures, continuity of care, individual productivity, personal preferences, and burnout risk, all while maximizing patients treated and minimizing unnecessary cost.
In this complexity, the market remains underserved and legacy actors fail to solve the problem. Forecasted patient arrivals are rarely modeled, alongside individual clinician productivity and the complex compensation models that exist.
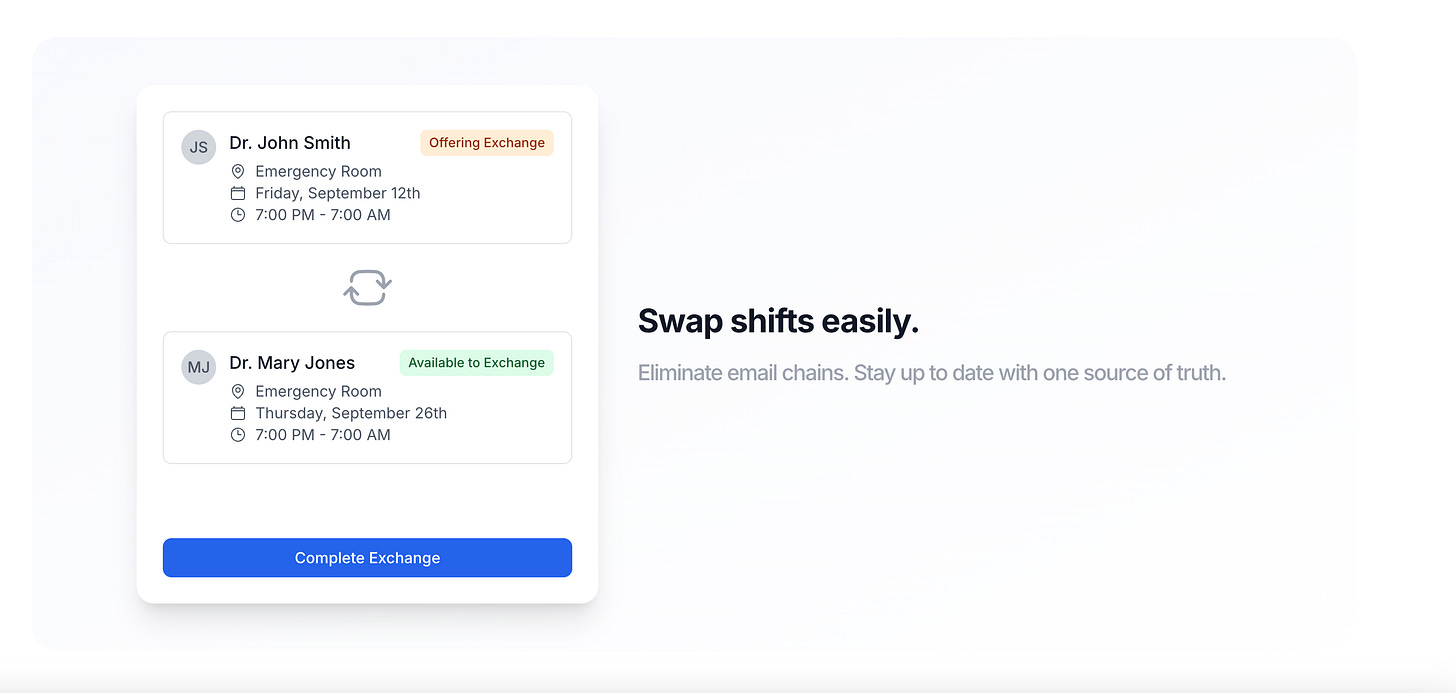
Second, workforce management is still fundamentally human-coordinated.
Currently, it is managed by full-time schedulers, administrative coordinators, department heads, or medical directors.
As a result, decisions become reactive and local. Trade-offs are resolved manually. Standards vary across sites. What should be a unified, system-level allocation problem is managed through individual judgment and coordination.
The infrastructure to support them does not exist. We believe it must.
Bulding Youshift
We decided to target heads on the healthcare labor shortage starting with solving staffing.
We are building an AI-native operating system to manage hospital workforce management at scale, starting with scheduling.
By optimizing internal labor first, and automating the process end-to-end, we establish the infrastructure layer. From there, payroll, compliance, hiring, and eventually external coordination become natural extensions.
Healthcare is complex. Procurement is slow. Compliance is strict. It would be easy to accept that this is simply the nature of healthcare, but structural pressure forces redesign.
Complexity is not a reason to avoid rebuilding infrastructure. It is the reason it hasn’t been rebuilt, and the reason it must be.
We believe workforce management is becoming the defining infrastructure challenge in healthcare. And we are building the system designed for it.
Hope this was valuable! Let me know if you’re investing in healthtech!
Cheers,
Guillermo
FAQs: The Future of Healthcare Workforce Management (Youshift)
1) What is the healthcare workforce shortage, and how bad is it?
Healthcare systems are running into a structural labor crunch: fewer clinicians available while demand rises. The article cites projections including 100,000+ physician and 200,000+ nurse shortages in the U.S. by 2033, alongside rising burnout and a rapidly aging population.
2) Why is healthcare staffing becoming a global infrastructure problem?
Because staffing isn’t just an HR task—it’s the operating constraint of care delivery. When hospitals can’t staff shifts, patient access, quality, and outcomes suffer, and the whole system becomes more expensive and reactive.
3) What are the biggest drivers of the healthcare labor crisis?
The piece highlights three reinforcing forces: shrinking clinician supply, expanding demand from aging populations, and labor costs becoming the dominant cost center (nearly ~60% of hospital operating costs, as stated in the article).
4) Why are hospitals spending so much on temporary clinicians (locums, travel nurses, etc.)?
When coverage gaps appear, hospitals buy short-term relief. The article notes $10B+ spent in the U.S. on temporary clinicians in one year, often at 30–50% higher per-shift costs.
5) Do temporary staffing markets make the shortage worse?
They can. Higher short-term pay pulls clinicians toward temporary work, while contractual restrictions can make it harder to convert those clinicians into full-time roles—fragmenting an already supply-constrained workforce (as described in the article).
6) What is “workforce management” in healthcare?
It’s the system that determines who works, when, at what cost, under what legal and contractual constraints—including scheduling, credentialing/compliance checks, payroll rules, and coverage requirements.
7) Why is hospital scheduling so hard to fix with standard software?
Because it’s a constrained, multi-objective optimization problem. A workable schedule must balance coverage, legal requirements, compensation models, continuity of care, preferences, productivity, and burnout risk—often across multiple sites and roles.
8) Why do hospitals still use spreadsheets and manual workarounds for scheduling?
The article argues that legacy tools weren’t built to handle today’s complexity—so humans “patch” the system with admin teams, manual coordination, and inconsistent standards that become reactive over time.
9) What does it mean that workforce management is “still human-coordinated”?
Key staffing decisions are often made by schedulers, department heads, and medical directors juggling trade-offs manually. That creates local, reactive decision-making instead of a unified system-level allocation approach.
10) How does poor staffing impact patient care and outcomes?
When staffing breaks, access breaks: delays, reduced throughput, inconsistent coverage, and clinician fatigue. The article also cites broader potential upside: solving the global shortage could reduce disease burden by enabling more timely access to essential services.
11) What is Youshift (sometimes written “Youshif”)?
In this article, Youshift is described as an AI-native operating system for hospital workforce management, starting with scheduling—aiming to optimize internal labor and automate staffing end-to-end.
12) What problem is Youshift solving first?
The first wedge is staffing and scheduling—because it is the daily operational bottleneck that drives labor costs, clinician experience, and patient access.
13) What does “AI-native operating system” mean in this context?
It means the core workflow is designed around automation and optimization from the ground up (not “AI added on” to old tools). In the article’s framing: model demand, account for constraints, and coordinate staffing decisions system-wide.
14) How does AI help reduce hospital labor costs without reducing care quality?
By optimizing internal labor (better coverage with existing teams), reducing overstaffing/understaffing, minimizing expensive last-minute coverage, and decreasing the need for premium-priced temporary shifts—while respecting compliance and continuity constraints.
15) Can better scheduling reduce clinician burnout?
That’s one of the central bets: schedules that respect preferences, fairness, rest rules, and workload distribution can reduce the constant “fire drill” dynamic that contributes to burnout (49% physician burnout is cited in the article).
16) Why start with emergency rooms and physician groups?
The article notes that ~60% of U.S. ERs are staffed by physician groups, and their profitability hinges on labor efficiency—making scheduling and workforce optimization especially high-leverage there.
17) What comes after scheduling in a workforce management platform?
The article frames scheduling as the foundation—then extending naturally into payroll, compliance, hiring, and eventually external coordination as a connected infrastructure layer.
18) What makes healthcare procurement and compliance harder than other industries?
Healthcare has strict compliance requirements, complex credentialing and labor rules, and slow procurement cycles. The article’s view is that these constraints are exactly why infrastructure needs a rebuild—not a reason to avoid it.
19) What ROI should hospitals look for from staffing optimization?
Operators typically look for reduced premium labor spend (e.g., temp clinicians), lower admin overhead, fewer last-minute coverage gaps, better clinician retention, and improved patient throughput. This aligns with the article’s emphasis on labor as the major cost center.
20) Who founded Youshift?
The piece introduces Lucía Vives (founder) and her two co-founders Jota Chamorro and Adolfo Roquero, who met at Harvard and set out to tackle workforce management as infrastructure.